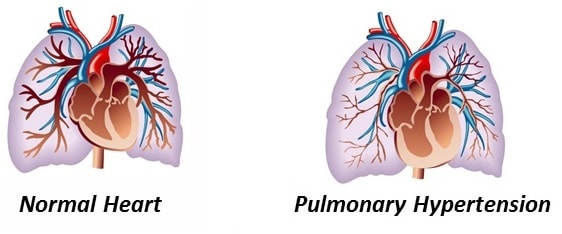
What is Pulmonary Hypertension?
Pulmonary hypertension means high pressures in the arteries of the lung often associated with pathological changes within the arterial wall. On one hand it may be a passive process due to volume or flow overload of pulmonary circulation sometimes reversible with the correction of underling cause such as left heart failure, hyperthyroidism, etc. On the other hand, PAH (Pulmonary arterial hypertension) is in situ disease of the arteries of the lung, almost always progressive leading to right heart failure or death if untreated.
Why is Pulmonary Hypertension Difficult to Diagnose?
Why is Pulmonary Hypertension Important to Recognize?
Are There Different Causes or Forms of Pulmonary Hypertension?
Current Challenges in Pulmonary Hypertension Diagnosis and Management
Our Solution
CVD Evaluator pulmonary hypertension module may serve as a clinical decision support system to aid providers in management of this somewhat mysterious, complex disease. The software is designed by the feedback of renowned PAH experts. It will assist in interpreting hemodynamic, echocardiographic data. It will bridge an individual profile to the literature for evidence based management choices.